We Do More
Doing more leads to better outcomes for our patients, partners, and staff. These improved outcomes include:

Our admissions teams do more work up-front to ensure a fast, smooth, and safe transition home.
We respond to referrals within one hour.
Our team-based, rigorous onboarding process helps us better understand our patient’s clinical needs and the family’s issues, challenges, and expectations up-front so we can provide better, more-sustainable care when the patient gets home. Issues related to housing, caregiving, and identifying the authorized representative are ideally resolved prior to discharge to ensure a safe and smooth transition home.
Non-negotiable clinical demands or expectations are uncovered up-front and addressed up-front. We encourage all appropriate family members to participate in the initial discussion of hospice to foster broad acceptance of hospice.
DME and critical medications are approved and delivered to the home prior to discharge. We are fully transparent about what hospice does and does not do.
We offer same-day discharges. We can accommodate quick SNF placements through positive and wide-ranging SNF relationships.

We say yes to more things to help families overcome their reluctance to hospice care.
Clinically progressive care allows us to bring patients onto hospice who are hospice-reluctant or who have non-negotiable clinical demands.
- IV Hydration
- IV/IM Antibiotics
- CPAP / Bi-Pap
- Paracentesis
- Thoracentesis
- Artificial Nutrition
- Challenging Wound Care
- Wound Vacs (Medicare Only)
- Pain Pumps
- High Flow Oxygen (up to 40 liters)

We provide more care and family education to ensure families feel comforted, supported and at peace.
Our staff visits the home, on average, four to five times per week, and often more as needed. Our hospice aides typically average three visits per week, but aide visits can be expanded to five times per week to meet the patient’s and family’s needs.
Families struggling with challenging dynamics or unexpected situations receive continuous education and devoted attention from the hospice interdisciplinary team. To help families who our struggling with their loved one’s disease process, we offer visits by physicians or nurse practitioners to answer their questions and concerns.
We know from experience that families often struggle with caring for their loved ones on nights and weekends. As such, our robust, compassionate, and responsive triage team skillfully provides after-hours care so our families are well-attended any time of day.
We work with a wound consultant who provides comprehensive wound care; we utilize labs to aid in symptom management; we offer podiatry visits to promote comfort; and we are generous with medical supplies.

We do more training with our staff so they are more skilled and confident, clinically but also in their ability to connect with families and help solve what brings them distress.
We believe that inspiring and dedicated people without strong clinical, patient-care, and customer service skills will not be able to make the impact they seek. As such, we are big believers in continuous and ongoing mentorship, training, and development.
We train our staff extensively so they are skilled and confident, clinically but also in their ability to think critically, solve challenging problems, resolve difficult issues, and connect with families. Our staff receive training across multiple platforms to ensure they are ready to provide outstanding care.
Staff receive, on average, two to three months of training.
Our training modalities include one-on-one training with a clinical manager, eLearning, classroom training, skills lab, mentorship, and shadowing.
We continually develop and update our own proprietary training materials so the material is engaging, fresh, and original.
We employ a large team of clinical managers, and our manager-to-staff ratios are among the best in the industry. This means more clinical direction, more mentorship, more support, and more ongoing training.

We have more clinical oversight to ensure we offer excellent care and excellent customer service, even in the face of clinical complexity, challenging family dynamics, and unexpected situations.
During regular hours, all patient and family calls into the office are directed to a clinical manager. This is a profoundly powerful difference because patients and families always have access to providers who can immediately address their issues.
We offer robust management ratios of one clinical manager to five registered nurse case managers. This means more clinical direction, more mentorship, more support, and more ongoing training. Additionally, our large team of clinical managers means that the clinical management team is very knowledgeable about each patient’s condition.
To ensure compliance and continuity of care, our clinical managers visit our SNF partners every month to ensure compliance with SNF requirements. Accordingly, we have not received a SNF deficiency since starting this process.
Lastly, a clinical manager is dedicated to overseeing all aspects of every admission—reviewing H&P, medication profile, and hospice eligibility—in coordination with hospice Medical Director.

Mi Amado

End-Stage Renal Disease
(ESRD)

Transitional Palliative Care
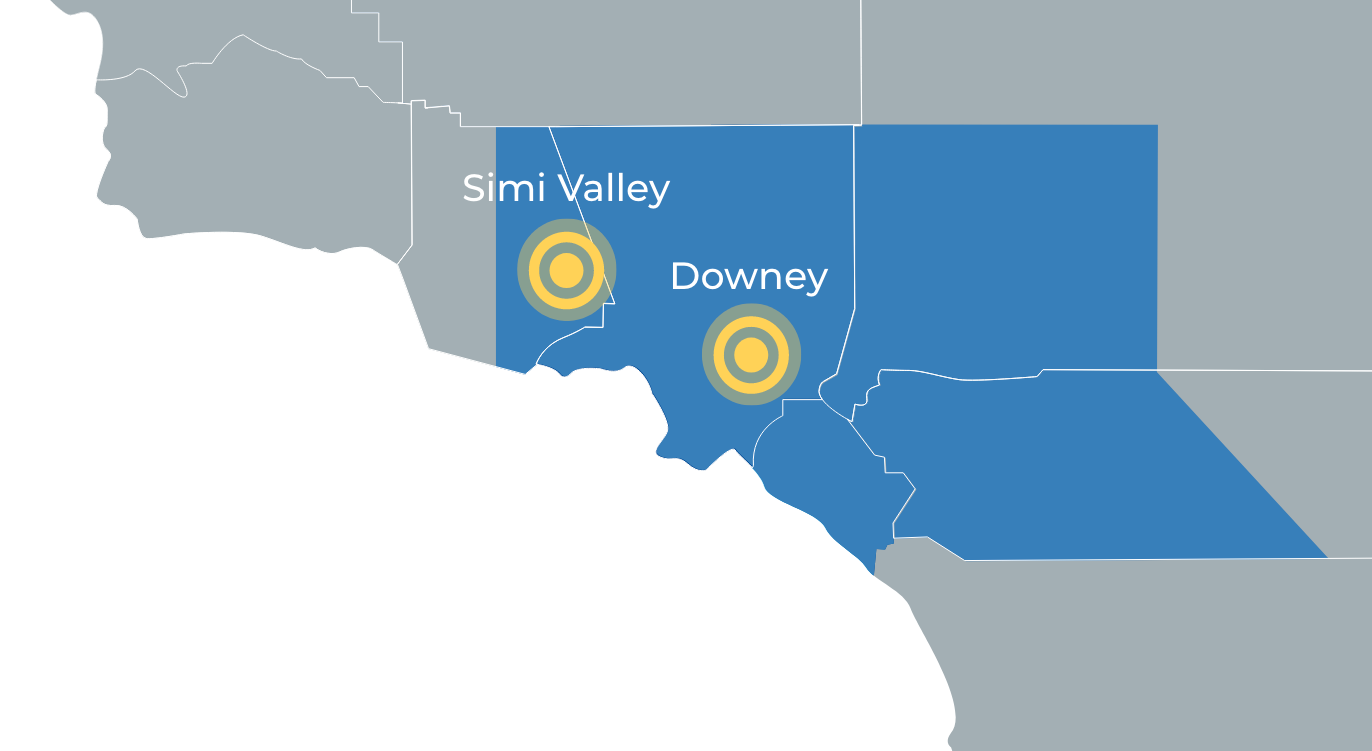
We cover more territory across Southern California.
Headquartered in Downey, we deliver care across Southern California markets with field a office in Simi Valley. Healing Care Hospice is Medicare-certified and accredited by the Accreditation Commission for Healthcare (ACHC).
See Our Service Areas & Locations